The Long COVID Road Ahead
We don't know what we don't know, but we are learning. And what we're learning is pretty alarming.
I think a lot about uncertainty. As a macroeconomist, that usually means I’m thinking about different economic and policy scenarios and how they might impact things like interest rates, inflation, consumer spending, business investment, unemployment, and so on. My spouse is a history professor. Among other things, he teaches a course on the global history of human health, and he writes about disease and epidemics. As you might imagine, we spend a lot of time talking about the pandemic and the economy.
The other day, we were talking about how lucky we’ve been. To the best of our knowledge, neither of us ever contracted COVID-19. We were fortunate to work from home for most of 2020 and part of 2021, and we were judicious about mask-wearing, especially before the whole family was fully vaccinated. Even with two teenagers and the lifting of mask mandates in their schools and in our university, it appears that we’ve all managed to avoid getting covid. Of course, we don’t know for sure. Uncertainty! It’s possible that one (or more) of us had an asymptomatic infection.
I hope not, and I hope we can avoid a breakthrough infection. It’s not just that I don’t want any of us to feel crummy for a short period of time. And, yes, I’m aware of the benefits of acquiring immunity through prior infection. But I’m worried about how much we still don’t know about the long-run damage—both human and economic—that comes from having COVID-19.
There’s so much we still don’t know. Data is being collected and evaluated by scientists and scholars the world over. I’m not equipped to evaluate medical research, but I try to stay broadly informed by paying attention to what the experts are telling us.
Yesterday, I listened to a panel of scholars present findings from a new white paper titled, "Long Covid’s Impact on Adult Americans: Early Indicators Estimating Prevalence and Cost.” The report was published by the Solve M.E. Initiative, a non-profit organization that focuses on post-infection diseases. It warns of a looming public health crisis — ”a mass debilitating event”— related to the incidence of long COVID.1
The figures are staggering, and I’m concerned that America is sleepwalking into this crisis.
Back in December 2020, Congress appropriated $1.15 billion to the National Institutes of Health (NIH) specifically for Long COVID research. But that’s a drop in the bucket, given the challenges that lie ahead.
The goal of the research was to estimate the prevalence and cost of Long COVID. Here are some of the key findings:
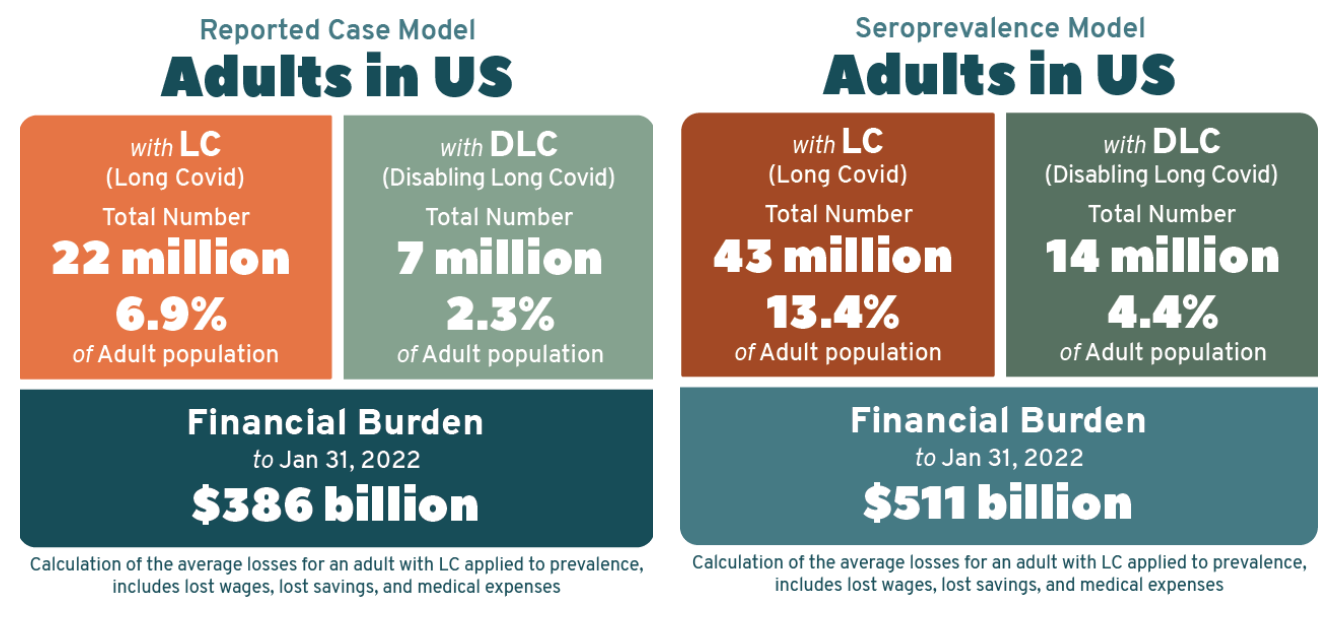
22 million U.S. adults are living with Long Covid (LC) – close to 7 percent of the population.
7 million are experiencing Disabling Long Covid (DLC) – 2.3 percent of the population.
As of January 2022, the cumulative cost of LC is estimated at more than $386 billion. (This estimate includes lost wages, lost savings, and medical expenses incurred by individuals. It does not include costs incurred by businesses or government agencies.)
To try to map out the scale of the problem we’re facing, researchers needed to figure out: (1) how many adults have been infected with COVID-19 (and survived) and (2) how likely it is for someone with a prior infection to develop Long COVID.2 There is obviously a degree of uncertainty in all of this. For example, we have official case counts, but we know that many cases went unreported.
The findings highlighted above rely on the official case count, together with an emerging consensus around the risk of developing Long COVID after infection. That consensus suggests that nearly one-third of people (30 percent) who become infected with COVID-19 will experience at least one lingering symptom six months later. Of those, about a third (10 percent) will report symptoms severe enough to interfere with work or activities of daily living, effectively rendering them with a disability.
As staggering as these numbers are, we know they can’t be right, because they exclude the cases that weren’t officially reported by the CDC. To adjust for this undercounting, researchers used data from the CDC’s Community Seroprevalence Survey, which draws inferences about the level of prior infection by gathering information about the prevalence of antibodies in communities across the US. When you do this, the number of people suffering from Long COVID basically doubles.
I encourage you to read the report or watch the researchers present their findings. I think it’s incredibly important stuff.
We are facing a mass disabling event. One way or another, it will impact all of us.
Women will be disproportionately burdened, as they leave the labor force to care for long haulers. The hardest hit will be those who were disproportionately impacted through the pandemic—black, indigenous, people of color. Employers will struggle to retain workers. In addition to the unimaginable toll this will take on tens of millions of our fellow Americans, there are implications for growth, productivity, inequality, etc.
In some respects, the pain we’re facing is already baked in. But there are things we can—and should—do to attenuate the human and economic dislocations that we know are coming.
Among other things, the white paper recommends that employers will need to be flexible, understanding that those suffering the effects of Long COVID will have good days and bad days. We need to make it easier for people to access Disability Insurance, to return to work when a string of good days allows, and to transition back onto disability when the inevitable bad days hit. We will need professional staff to assist those who need legal representation and support for those navigating the disability system—case managers/advocates/etc.
President Biden’s Build Back Better agenda would have helped to fund some of the investments we so desperately need in care work. But, thanks to Sen. Manchin (D-WV), that isn’t happening. Heck, it isn’t even clear that Congress will continue to provide funding for vaccines and treatments. (Click to read the thread.)
It’s all pretty depressing stuff. I hope things will change. It’s always darkest before the dawn.
Long COVID is a post-infection illness that refers to lingering symptoms that persist six or more months after initial infection. People with Long Covid can experience a broad range of symptoms, some of which can be disabling enough to prevent a return to work or recovery to pre-infection health.
Most people who develop long-COVID had mild or asymptotic cases.





I subscribe to your optimism and MMT expertise but our identity politics will continue to produce harmful policies and keep us from realizing the Great Society. Thank you so much. I will keep the Faith.
Thought of this subject while listening to criticism of China's "extreme" zero Covid policy. China has 1.4 B people and the WHO has China at 1.032 M cases (wow that seems low) and 15 K deaths. And politicians ruminate about being competitive with China? Think about what this means vis a vis long Covid.
Also: during the video the advice is to incentivize business to "be flexible" with people who suffer from long Covid. No. Absolutely not. They need to be told what they will do because otherwise, they won't do it. But still take the incentive. Let's not be naive.
Finally, the word is "overhaul" with respect to the disability system. Not hire lawyers. Scrap and rebuild. No time for putting lipstick on a pig.